Key Takeaways
- Post-surgical lymphatic massage helps move trapped fluid after procedures like liposuction, tummy tuck, and BBL, reducing swelling and preventing hard scar tissue from forming.
- This specialized technique is different from spa massage—it requires certified training in Manual Lymphatic Drainage (MLD) and close coordination with your surgeon’s recovery plan.
- Most patients need 3–10 sessions starting within the first week after surgery, paired with medical-grade compression garments for the best results.
Why Your Body Needs Help Moving Fluid After Surgery
Surgery disrupts the delicate network of vessels that normally drain fluid from your tissues. When your surgeon performs any body contouring procedure such as: liposuction, removes skin during a tummy tuck, or sculpts areas during a Brazilian Butt Lift, those pathways get interrupted.
Your body responds by sending fluid to the area to start healing. That’s normal and necessary. But without those drainage routes working properly, the fluid has nowhere to go. It pools in the spaces between your tissues, causing swelling, tightness, and discomfort.
Left alone, that protein-rich fluid can harden into thick, fibrous scar tissue—what we call fibrosis. This is what creates lumps, uneven contours, and that “tight” feeling that lingers for months.
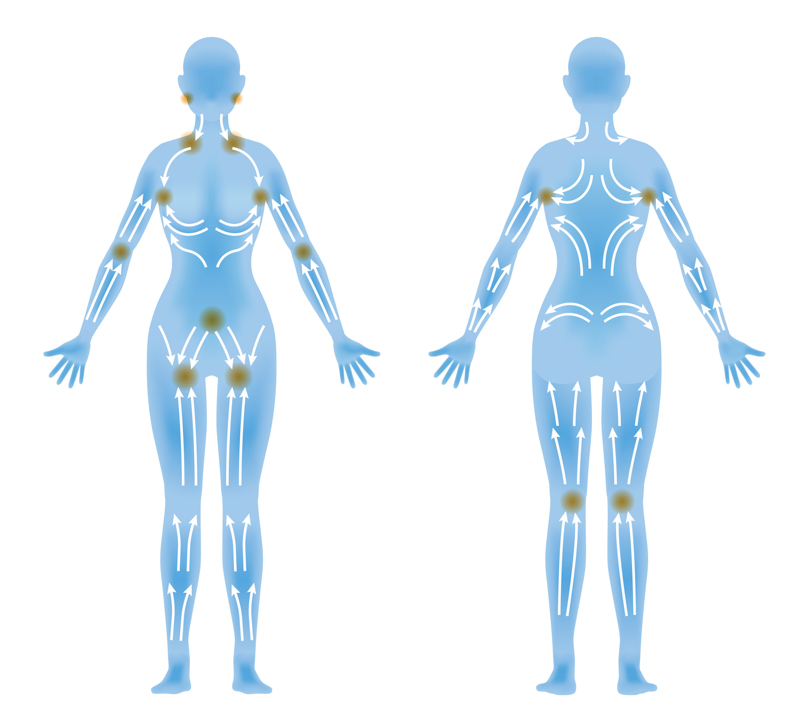
Post-surgical lymphatic massage gives your body a gentle assist. It manually moves that trapped fluid toward working lymph nodes so your system can filter it out naturally.
What Makes Lymphatic Massage Different from Regular Massage
If you’ve had a spa massage before, this will feel completely different.
Regular massage uses firm pressure to work out muscle tension. Post-surgical lymphatic drainage uses extremely light, rhythmic strokes—just enough pressure to stimulate the surface vessels under your skin without disturbing healing tissue or causing pain.
The technique is called Manual Lymphatic Drainage, or MLD. It was originally developed to treat lymphedema, a condition where the lymph system is damaged or blocked. Certified therapists trained in MLD understand the anatomy of your lymphatic system and how to work around incisions, drains, and areas of trauma.
This is not something you should trust to just anyone. Your therapist should be MLD-certified and experienced in post-operative care. They should also communicate directly with your surgeon to follow your specific recovery protocol.

How Your Lymphatic System Supports Healing
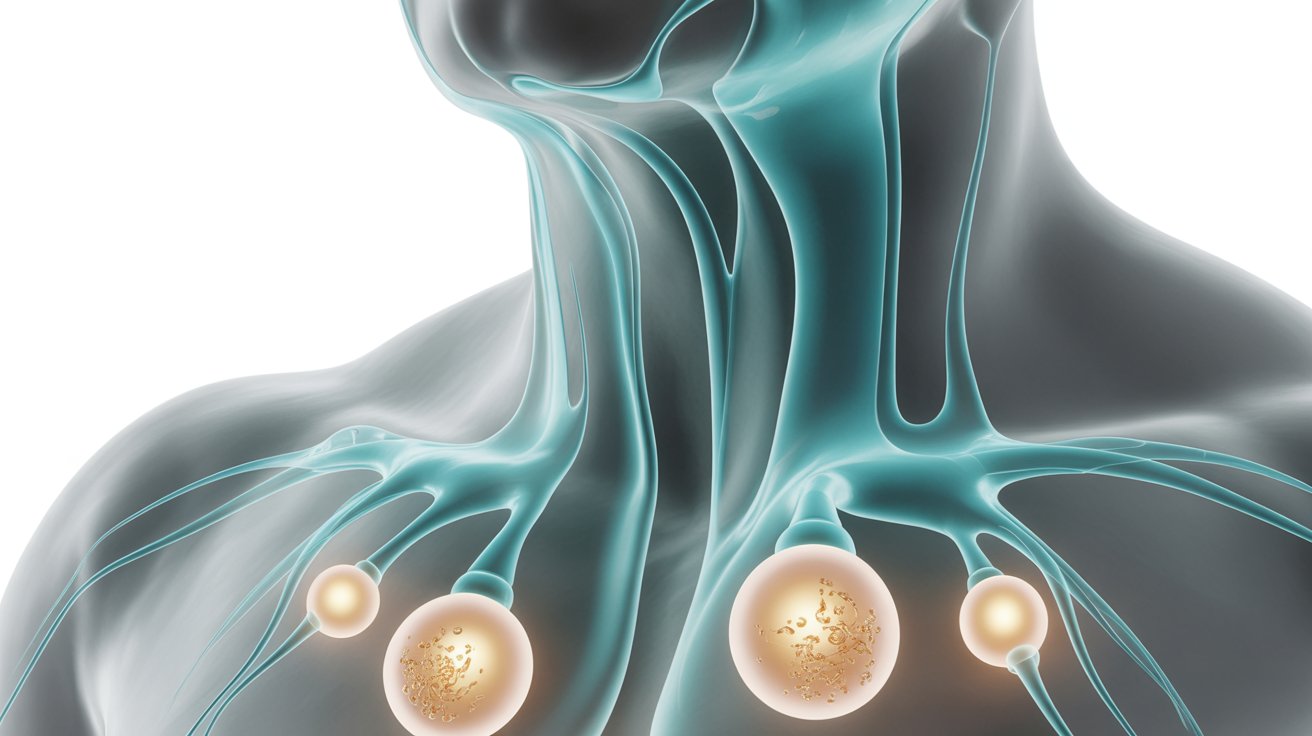
Your lymphatic system is part of your immune system. It’s a network of vessels and nodes that filters waste, fights infection, and keeps fluid levels balanced throughout your body.
Lymph fluid is clear and carries proteins, metabolic waste, and white blood cells called lymphocytes. Lymph nodes act as filtration stations, removing toxins and circulating clean fluid back into your bloodstream.
When you’re under physical stress—like recovering from surgery—your lymphatic system works overtime. But if the vessels are damaged or blocked by swelling, the system can’t keep up. That’s when you see persistent puffiness, bruising that won’t fade, and areas that feel thick or lumpy.
Manual lymphatic drainage helps restart that flow, supporting your body’s natural healing process.
What Happens During a Session
Your first session will likely happen within the first week after surgery, once your surgeon gives clearance. Every case is unique, so timing depends on your procedure, how much swelling you have, and whether you have drains in place.
Your therapist will ask about your surgery, check your incisions, and assess areas of swelling. The actual massage uses slow, gentle, wave-like motions that follow the direction of lymph flow toward your nodes.
You might notice fluid leaking from incision sites during or after the session. That’s normal—it means the massage is working. Your therapist may also use light compression or positioning to help gravity assist drainage.
Sessions typically last 30–60 minutes. Most patients describe it as soothing, not painful. If you feel sharp pain or intense discomfort, let your therapist know immediately.
How Many Sessions You’ll Need
The number of sessions depends on the type and extent of your surgery.
For smaller procedures like a mini tummy tuck or facial surgery, you might need 3–5 sessions. For more invasive body contouring—like Lipo 360, full abdominoplasty, or BBL—plan for 6–10 sessions or more.
Timing matters, too. The acute phase (the first 1–2 weeks) is when swelling peaks and your body is most responsive to drainage. Sessions during this window are often scheduled every 1–3 days.
As you move into the sub-acute phase (weeks 3–6), sessions typically shift to once or twice a week. Some patients continue maintenance sessions for 2–3 months to address residual swelling or prevent fibrosis.
Your therapist and surgeon will create a schedule based on how your body is responding. If you develop a seroma (a pocket of fluid) or early signs of hardness, they may recommend more frequent sessions.
Compression Garments Work Hand-in-Hand with Massage
Lymphatic massage is most effective when paired with medical-grade compression garments.
These garments apply consistent, gentle pressure to surgical areas, preventing fluid from pooling and helping tissues adhere as they heal. They also reduce the risk of seromas, support your new contours, and minimize scar tissue formation.
You’ll start with a Stage 1 garment immediately after surgery. These are designed to accommodate initial swelling and are typically worn 24/7 for the first few weeks, except during showers and massage sessions.
Around week 3 or 4, as swelling begins to resolve, you’ll transition to a smaller, firmer Stage 2 garment. This provides more targeted compression and is usually worn for an additional 3–6 weeks.
Your surgeon will give you specific instructions on when to wear your garment, how tight it should feel, and when to switch stages. Follow those instructions closely—skipping compression or stopping too early can undo the benefits of your massage sessions.

What Fibrosis Is and How to Prevent It
Fibrosis is the development of thick, hard scar tissue under the skin. It happens when protein-rich fluid sits in your tissues too long and your body lays down dense collagen to “wall it off.”
You’ll feel it as firm lumps, rope-like bands, or areas that don’t soften when you press on them. Fibrosis is more common after liposuction, especially in areas where a lot of fat was removed or where multiple passes were made with the cannula.
The best way to prevent fibrosis is early, consistent lymphatic drainage combined with compression. If you start to notice hard spots forming, let your therapist and surgeon know right away. Techniques like ultrasound therapy or radiofrequency can sometimes help break up early fibrosis, but they work best when started early.
Every case is unique, and some degree of firmness is normal during healing. But if areas aren’t softening after several weeks, that’s a sign you need more support.
Red Flags: When to Call Your Surgeon
Lymphatic massage is safe when performed by a trained professional following your surgeon’s protocols. But there are times when you should pause and reach out to your surgical team.
Contact your surgeon if you notice:
- Sudden increase in swelling, especially if it’s one-sided or painful
- Redness, warmth, or streaking around incisions
- Fever or chills
- Foul-smelling drainage or pus
- A firm, fluid-filled pocket that appears suddenly (possible seroma)
- Pain that’s getting worse instead of better
These could be signs of infection, hematoma, or other complications that need medical attention. Your massage therapist is part of your recovery team, but they are not a substitute for your surgeon’s care.
Supporting Your Recovery at Home

Between sessions, there are simple things you can do to support lymphatic drainage.
Stay hydrated. Your lymph system needs water to move fluid efficiently. Aim for at least 8 glasses a day unless your surgeon advises otherwise.
Move gently. Light walking encourages circulation without straining healing tissues. Avoid vigorous exercise, heavy lifting, or anything that spikes your heart rate until your surgeon clears you.
Elevate when possible. Keeping surgical areas elevated (especially legs after lipo or BBL) helps gravity assist drainage and reduces pooling.
Wear your garment as directed. Consistency matters. If your garment is too loose, too tight, or uncomfortable, talk to your surgeon—don’t just stop wearing it.
Eat a balanced diet rich in protein and vitamins to support tissue repair. Some patients find that supplements like arnica or bromelain help with bruising, but check with your surgeon before adding anything new.
Who Should Not Have Lymphatic Massage
Lymphatic drainage is generally safe, but it’s not appropriate for everyone.
You should not have lymphatic massage if you have:
- Active infection or fever
- Blood clots or a history of deep vein thrombosis (DVT)
- Congestive heart failure or kidney failure
- Cancer that has spread to the lymph nodes (unless cleared by your oncologist)
- Open wounds or unhealed incisions
If you have drains in place, your therapist may work around them or wait until they’re removed, depending on your surgeon’s preference.
Always disclose your full medical history to both your surgeon and your massage therapist so they can create a safe, effective plan for you.
What to Do Next
If you’ve recently had cosmetic surgery or are planning a procedure, ask your surgeon about post-operative lymphatic drainage during your consultation. Many practices can refer you to certified therapists they trust, or they may offer sessions in-house.
If you’re already in recovery and experiencing swelling, hardness, or uneven contours, it’s not too late to start. Even a few weeks post-op, lymphatic massage can still make a meaningful difference.
Our team works closely with board-certified plastic surgeons throughout the area to support safe, smooth recoveries. If you’d like to schedule a session or have questions about whether lymphatic drainage is right for you, reach out—we’re here to help you heal well.


 Typical Recovery Timelines After Plastic Surgery
Typical Recovery Timelines After Plastic Surgery